Leads ECG Placement: 7 Critical Mistakes to Avoid Now!
Understanding leads ecg placement is crucial for accurate heart diagnostics. A small error can lead to misdiagnosis. Let’s dive into the essentials every healthcare provider must know.
What Is Leads ECG Placement and Why It Matters

Leads ecg placement refers to the precise positioning of electrodes on the body to record the heart’s electrical activity. This process is fundamental in electrocardiography, a non-invasive test used globally to assess cardiac function. Incorrect placement can distort the waveform, leading to inaccurate interpretations and potentially dangerous clinical decisions.
The Science Behind ECG Leads
An ECG machine uses 12 standard leads—comprising limb leads, augmented limb leads, and precordial (chest) leads—to capture the heart’s electrical signals from different angles. Each lead provides a unique view of the myocardium, enabling clinicians to detect abnormalities such as arrhythmias, ischemia, or infarction.
- Limb leads (I, II, III) measure electrical activity in the frontal plane.
- Augmented limb leads (aVR, aVL, aVF) offer additional frontal plane perspectives.
- Precordial leads (V1–V6) focus on the horizontal plane, particularly the left ventricle.
Proper leads ecg placement ensures that these views are anatomically accurate. According to the American Heart Association (AHA), even a 20 mm displacement of a precordial electrode can alter the ECG significantly, mimicking conditions like myocardial infarction.
“Accurate electrode placement is the cornerstone of a reliable ECG interpretation.” – American Heart Association, 2020 Guidelines
Common Misconceptions About Leads ECG Placement
Many clinicians assume that approximate placement is sufficient, especially in emergency settings. However, research published in the Journal of the American College of Cardiology shows that up to 40% of ECGs have at least one lead misplaced, often going unnoticed.
- Misconception: Chest leads can be estimated by eye.
- Fact: Anatomical landmarks must be palpated, not guessed.
- Misconception: Limb leads can be placed anywhere on the limbs.
- Fact: They should be placed distally on the wrists and ankles to reduce noise and artifact.
Another common error is reversing the right and left arm electrodes, which can invert lead I and create a false impression of dextrocardia. This is a classic example of how a simple mistake in leads ecg placement can lead to a cascade of diagnostic errors.
Anatomical Landmarks for Correct Leads ECG Placement
Accurate ECG interpretation begins with correct electrode positioning based on anatomical landmarks. These landmarks serve as reference points to ensure consistency across recordings and providers. Mastery of these landmarks is essential for both novice and experienced practitioners.
Locating the V1 and V2 Positions
The placement of leads V1 and V2 is among the most critical in the entire ECG setup. These electrodes are positioned in the fourth intercostal space, just to the right and left of the sternum, respectively.
- V1: Fourth intercostal space, right sternal border.
- V2: Fourth intercostal space, left sternal border.
To locate the fourth intercostal space, start by identifying the angle of Louis (sternal angle) at the second rib. Move your fingers down to the second intercostal space, then slide laterally to feel the third rib, and finally drop down to the fourth intercostal space. Misplacement above or below this level can shift the QRS axis and mimic right or left ventricular hypertrophy.
“Palpation beats estimation every time.” – Dr. William A. Zoghbi, Echocardiography Expert
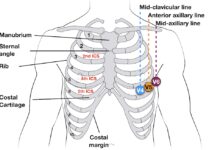
Positioning V3 to V6 Across the Chest
After placing V1 and V2, the remaining precordial leads (V3–V6) are positioned in a horizontal line across the chest.
- V3: Midway between V2 and V4.
- V4: Fifth intercostal space at the midclavicular line.
- V5: Same horizontal level as V4, at the anterior axillary line.
- V6: Same level as V4 and V5, at the midaxillary line.
It’s crucial to maintain the same horizontal plane for V4–V6. Placing V4 too high or too low can distort the R-wave progression, leading to misinterpretation of anterior myocardial infarction. A study in NCBI found that incorrect V4 placement was the most common error, occurring in nearly 30% of routine ECGs.
Step-by-Step Guide to Proper Leads ECG Placement
Performing an ECG with precision requires a systematic approach. Following a standardized protocol minimizes variability and enhances diagnostic accuracy. Here’s a detailed, step-by-step method for correct leads ecg placement.
Preparing the Patient and Equipment
Before placing any electrodes, ensure the patient is relaxed and lying flat. Remove any clothing that obstructs electrode placement. Clean the skin with alcohol wipes to reduce impedance and improve signal quality, especially in patients with oily or hairy skin.
- Use conductive gel or pre-gelled electrodes for better contact.
- Shave excessive chest hair if necessary to ensure adhesion.
- Check electrode expiration dates and integrity.
Position the ECG machine at the head of the bed for easy access. Confirm that all leads are properly connected and the machine is calibrated. This preparation phase is often rushed but is vital for high-quality tracings.
Sequential Electrode Placement Protocol
Follow this sequence to avoid confusion and ensure accuracy:
- Place V1 and V2 first using anatomical landmarks.
- Locate V4 by finding the fifth intercostal space at the midclavicular line.
- Place V3 midway between V2 and V4.
- Place V5 at the anterior axillary line, same horizontal level as V4.
- Place V6 at the midaxillary line, same level as V4 and V5.
- Attach limb electrodes: RA (right arm), LA (left arm), RL (right leg), LL (left leg).
The limb electrodes are typically placed on the distal limbs—wrists and ankles. While some protocols allow placement on the upper arms and thighs, consistency is key. Avoid placing limb leads on the torso, as this can alter the electrical baseline.
“Standardization is not bureaucracy—it’s the foundation of clinical reliability.” – European Society of Cardiology
Common Errors in Leads ECG Placement and How to Fix Them
Despite its routine nature, leads ecg placement is fraught with errors. Many of these mistakes are preventable with proper training and attention to detail. Recognizing and correcting them is essential for diagnostic accuracy.
Incorrect Precordial Lead Placement
One of the most frequent errors is misplacing the precordial leads, especially V1 and V2. Placing them in the third or fifth intercostal space can mimic right bundle branch block or anterior infarction.
- Solution: Always palpate the sternal angle to locate the second rib, then count down to the fourth intercostal space.
- Use a measuring tape or ECG placement guide for consistency.
- Double-check V4 placement at the fifth intercostal space, midclavicular line.
A 2021 study in Heart Journal found that using a standardized placement template reduced errors by 65% in emergency departments.
Limb Lead Reversal and Its Consequences
Reversing the right and left arm electrodes is a common but serious error. This swap inverts lead I and aVL, and can make lead II resemble lead III, leading to misdiagnosis of axis deviation or dextrocardia.
- Signs of reversal: Negative P wave in lead I, aVR positive, aVL negative.
- Fix: Recheck electrode labels and reattach correctly.
- Prevention: Use color-coded leads and train staff regularly.
Limb lead reversals are often missed during interpretation, especially if the clinician is unaware of the possibility. Always inspect the ECG for clues before making a diagnosis.
Special Considerations in Leads ECG Placement
Certain patient populations and clinical scenarios require modifications to standard leads ecg placement. These adaptations ensure diagnostic accuracy while maintaining patient comfort and safety.
ECG Placement in Obese or Anatomically Challenging Patients
In obese patients, the standard intercostal spaces may be difficult to palpate. Excess adipose tissue can obscure bony landmarks, leading to inaccurate electrode placement.
- Use ultrasound guidance in extreme cases to locate anatomical structures.
- Apply firm pressure with fingers to feel through soft tissue.
- Consider using longer electrode leads or extensions for better reach.
For patients with chest deformities (e.g., pectus excavatum), the heart’s position may be altered. In such cases, documenting the modified placement is crucial for future comparison.
Alternative Lead Placements in Critical Care
In intensive care units, patients often have IV lines, dressings, or monitoring devices that obstruct standard lead positions. Alternative placements may be necessary.
- Limb leads can be placed on the upper arms and thighs if distal sites are unavailable.
- Ensure all limb electrodes are placed symmetrically to avoid baseline shifts.
- Document any deviations from standard placement on the ECG report.
While modified placements are acceptable, they should be clearly noted, as they can affect waveform morphology. The AHA recommends that any non-standard placement be labeled to prevent misinterpretation.
Impact of Leads ECG Placement on Diagnosis
The accuracy of ECG interpretation is directly tied to the quality of the recording, which in turn depends on correct leads ecg placement. Even minor deviations can produce changes that mimic life-threatening conditions.
Mimicking Myocardial Infarction
Incorrect placement of V1–V3 can create the appearance of anterior ST-segment elevation, suggesting acute myocardial infarction. This can lead to unnecessary activation of the cath lab and invasive procedures.
- Example: If V1 is placed too high, it may show ST elevation resembling anterior MI.
- Differentiation: Check for reciprocal changes, clinical symptoms, and troponin levels.
- Best practice: Repeat ECG with correct placement if suspicion of artifact exists.
A case report in European Heart Journal described a patient who was nearly taken to angiography due to a misplaced V2 electrode causing false ST elevation.
Altering Cardiac Axis and R-Wave Progression
Improper lead positioning can shift the electrical axis and disrupt R-wave progression across the precordial leads.
- Rightward axis shift: Can occur with reversed arm electrodes.
- Poor R-wave progression: Often due to high or low placement of V3–V5.
- Clinical implication: May be mistaken for old anterior infarction or conduction abnormalities.
Always assess R-wave progression from V1 to V6. A normal progression shows increasing R-wave amplitude. Any deviation should prompt a review of lead placement before concluding pathology.
Training and Quality Assurance in Leads ECG Placement
Ensuring consistent, accurate leads ecg placement requires ongoing education and quality control. Hospitals and clinics must implement training programs and audit systems to maintain high standards.
Effective Training Programs for Healthcare Staff
Not all staff who perform ECGs are cardiologists. Nurses, technicians, and emergency responders must be trained in proper technique.
- Use hands-on workshops with mannequins and real-time feedback.
- Incorporate ECG placement into annual competency assessments.
- Provide visual aids and quick-reference guides at point of care.
Simulation-based training has been shown to improve accuracy by up to 50%, according to a study in BMC Medical Education.
Implementing ECG Quality Audits
Regular audits of ECG tracings can identify systemic placement errors and drive improvement.
- Review a random sample of ECGs monthly for lead placement accuracy.
- Use a checklist based on AHA/ESC guidelines.
- Provide feedback to staff and retrain as needed.
Hospitals with formal ECG audit programs report fewer diagnostic errors and higher staff confidence. Quality assurance is not punitive—it’s a tool for excellence.
What happens if ECG leads are placed incorrectly?
Incorrect leads ecg placement can distort the ECG waveform, leading to misdiagnosis of conditions like myocardial infarction, arrhythmias, or axis deviation. It may result in unnecessary tests, treatments, or missed diagnoses.
How can I ensure accurate V1 and V2 placement?
Palpate the sternal angle (angle of Louis) to locate the second rib, then count down to the fourth intercostal space. V1 goes on the right sternal border, V2 on the left. Use anatomical landmarks, not estimation.
Can limb leads be placed on the torso?
While limb leads can be placed on the upper arms and thighs in certain situations, they should not be placed on the torso itself. Doing so alters the electrical reference and can distort the ECG. Always maintain consistency and document any deviations.
Does patient position affect ECG results?
Yes, patient position can influence ECG morphology. The standard is supine, but changes in posture (e.g., sitting, standing) can shift the cardiac axis. Always record the patient’s position and keep it consistent for serial comparisons.
Are there tools to assist with leads ecg placement?
Yes, tools like ECG placement templates, anatomical guides, and even smartphone apps can help ensure accuracy. Some hospitals use ultrasound to confirm electrode placement in challenging cases.
Accurate leads ecg placement is not just a technical step—it’s a critical component of cardiac diagnosis. From understanding anatomical landmarks to avoiding common errors, every detail matters. By following standardized protocols, training staff effectively, and conducting quality audits, healthcare providers can ensure reliable ECG results. Remember, a well-placed lead can mean the difference between life and death. Mastering leads ecg placement is a skill worth perfecting.
Further Reading: